The Skin Microbiome
Recently I came across a paper published in Microorganisms, which piqued my interest. This paper suggests that the catastrophic loss in environmental biodiversity is replicated on the skin microbiome, and this reduction in diversity may be a substantial factor contributing to the rise in chronic diseases (Wallen-Russell, et al., 2023).
It has been understood for some time that the skin microbiome plays a crucial role in maintaining healthy skin by fostering a balanced ecosystem which supports the skin’s barrier function and immune response. A diverse skin microbiome helps regulate inflammation, ward off harmful pathogens, and promote overall skin resilience. Loss of skin microbiome stability (dysbiosis) has been linked with acne, eczema, psoriasis, rosacea, body odour, tinea and a host of other skin conditions.
What I found interesting about the Wallen-Russell (2023) paper is the assertion that skin biodiversity loss is not just contributing to skin conditions but could also play a causal role in overall chronic disease development. This biodiversity decline could also be influencing systemic health issues such as food allergies, asthma, cardiovascular diseases, and Parkinson's disease. And, parallel to a loss of diversity in the skin microbiome, is frequently a loss of diversity in the gut microbiome.
Gut health has long been a focus of naturopathic approaches for skin issues and indeed other chronic health issues. Known as the gut-skin axis, this relationship underscores how disruptions in the gut microbiome, known as dysbiosis, can influence skin health, potentially leading to or exacerbating dermatological conditions. The focus has usually been how the gut affects the skin, for example how sugar intake can cause dysbiosis and lead to exacerbations of acne or how antibiotic use during infancy can increase the risk of atopic dermatitis (Wallen-Russell, et al., 2023). The ways the gut interacts with the skin are numerous and include the following (Mahmud, et al., 2022):
Immune System Modulation: The gut microbiome plays a crucial role in shaping the body's immune responses. An imbalance in gut bacteria can lead to systemic inflammation, which may manifest in the skin as conditions like acne, psoriasis, or atopic dermatitis.
Metabolic Byproducts: Gut bacteria produce metabolites, such as short-chain fatty acids (SCFAs), that have systemic effects. These metabolites can influence skin barrier function and inflammation levels.
Microbial Translocation: In cases of increased intestinal permeability, often referred to as "leaky gut," microbial components can enter the bloodstream and affect distant organs, including the skin, potentially triggering inflammatory skin conditions.
However, this is not just a one-way street. For example, food allergies are now thought to be contributed to by exposure to food through damaged skin and disruptions to the skin barrier – a case of “leaky skin”. Emerging is the idea that reductions in skin diversity also contribute to diminished gut microbiome diversity, a negative feedback loop that further impacts gut issues and perhaps, wider systemic issues?
What happens on the skin doesn’t always stay there!
The skin is the body’s first line of defence against external pathogens, and the microbiome acts as a key player in this protective function. A diverse microbiome supports the skin's ability to fend off harmful microorganisms by competing for resources and space. When microbial diversity declines, pathogenic organisms are more likely to dominate, weakening the skin's defence mechanisms and creating pathways for infections, bacterial translocation (bacteria spreading from the skin into systemic circulation) and chronic inflammation.
Chronic inflammation is a well-documented precursor to many systemic diseases and individuals with reduced skin microbiome diversity often exhibit heightened inflammatory markers, which can exacerbate conditions like psoriasis and lupus. This chronic inflammation may not remain localised; it can enter systemic circulation, potentially contributing to diseases such as rheumatoid arthritis and inflammatory bowel disease.
Skin dysbiosis may also affect neurological health through the skin-brain axis. This bi-directional communication system links the skin, nervous system, and immune system. Disruptions in the skin microbiome can influence neuroinflammatory pathways, potentially contributing to neurodegenerative diseases like Parkinson’s and Alzheimer’s disease.
While this sounds like a remote possibility, studies have indicated that systemic inflammation caused by microbial imbalances can cross the blood-brain barrier, contributing to neuroinflammation. Most often, research is focused on gut microbial translocation to the brain but again, things don’t always stay where they are meant to and if skin bacteria translocate to systemic circulation, then this becomes a possibility. And given that chronic skin conditions like eczema and psoriasis have been associated with increased risks of mental health issues, including anxiety and depression (likely due to the impact of systemic inflammation and immune activation on brain chemistry), perhaps the possibility is not so remote.
The decline in skin microbial diversity has also been linked to the global increase in allergic conditions such as food allergies, asthma, and atopic dermatitis. A less diverse microbiome can impair the skin's ability to regulate immune responses, leading to hypersensitivity and increased allergic reactions. Autoimmune disorders, where the immune system mistakenly attacks healthy tissue, are also thought to be influenced by microbial imbalances. For example, recent studies have found that individuals with conditions like lupus often show distinct microbiome profiles, including reduced skin and gut diversity.
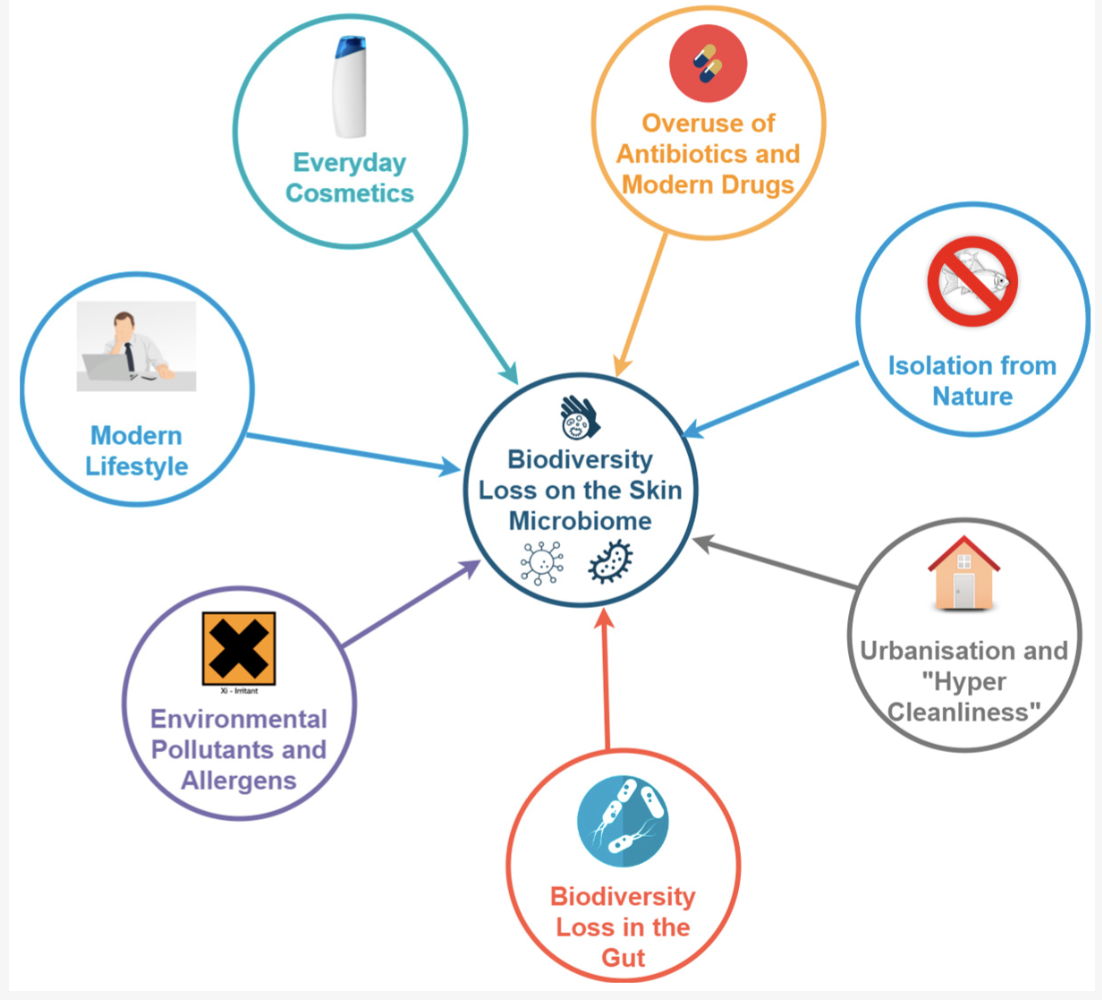
There are a host of factors that have the potential to induce skin dysbiosis (McLoughlin, et al., 2022):
Antibiotics – long term topical use in acne has led to bacterial resistance and loss of beneficial bacteria, allowing pathogenic species to flourish
Hygiene measures – over cleaning and the use of anti-microbial products such as hand sanitisers and antiseptic wipes. This has been hypothesised as one of the factors leading to a loss of immune tolerance and prevalence of atopic dermatitis.
Personal care products – the number of soaps, cosmetics, steroid medications shift the skin’s natural microbiota. Specifically, products that contain preservatives (e.g. izothiasoline), alcohol, paraffins and fragrances can lead to skin dysbiosis.
Skin pH – the surface of the skin, known as the acid mantle, helps maintain a healthy skin ecosystem. There is a positive relationship between the pH of the skin (5 being optimal) and healthy skin microflora. Using cleansers (soap, body wash etc) or applying alkaline moisturisers can impact the skin pH, particularly where skin is already damaged e.g. eczema.
This list is not exhaustive and other factors, such as isolation from nature, can be seen in the diagram below:
(Wallen-Russell, et al., 2023)
Aiming to restore a healthy skin microbiome by minimising disruptors and restoring skin pH and protective function is a naturopathic focus when addressing chronic skin conditions within clinical practice.
A Broader Perspective on Dysbiosis
The implications of skin microbiome dysbiosis highlight a broader theme: the interconnectedness of human health systems. As the Microorganisms study suggests, disruptions in the skin microbiome can cascade into systemic imbalances, emphasising the need for an approach that doesn’t just focus on the specific organ or tissue affected. It is critical to take a holistic approach to healthcare, one that looks at the interconnectedness of our body and the environment around us.
If are interested in booking for a consultation or have any questions please reach out via the contact page or let me know if you prefer a phone call and we can have a chat.
References
Mahmud, M. R., Akter, S., Tamanna, S. K., Mazumder, L., Esti, I. Z., Banerjee, S., ... & Pirttilä, A. M. (2022). Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut microbes, 14(1), 2096995.
McLoughlin, I. J., Wright, E. M., Tagg, J. R., Jain, R., & Hale, J. D. (2022). Skin microbiome—the next frontier for probiotic intervention. Probiotics and antimicrobial proteins, 14(4), 630-647.
Wallen-Russell, C., Pearlman, N., Wallen-Russell, S., Cretoiu, D., Thompson, D. C., & Voinea, S. C. (2023). A Catastrophic Biodiversity Loss in the Environment Is Being Replicated on the Skin Microbiome: Is This a Major Contributor to the Chronic Disease Epidemic?. Microorganisms, 11(11), 2784.