A holistic approach to chronic pain
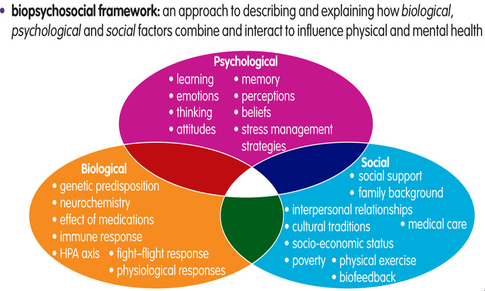
An article in the Australian Pain Newsletter by pain specialist Dr Chris Hayes (2016) really stood out to me recently as it emphasises the necessity for a holistic approach to the management of chronic non-cancer pain. The biopsychosocial model is widely accepted as the predominant framework for understanding the experience of chronic pain and its negative consequences, and is supported by a large body of research. The model takes a broad and holistic view of the factors that contribute to chronic pain and the interaction of biological (genetic, biochemical, trauma), psychological (mood, behaviour) and social factors (familial, medical, work place etc) and was developed to counter the biomedical model, which suggests that disease is the result of only biological factors.
While the biopsychosocial model is considered best practice, there is a lack of awareness within both the healthcare system and broader community and as such a biomedical approach to treatment often predominates. The upshot is that optimal treatment options aren’t available to those in chronic pain and the focus on structures, diagnosis, medications and invasive treatments is continued without widening treatment options (Hayes, 2016).
The key to patient’s accessing treatment based on the biopsychosocial model is the awareness that individual treatment will encompass an integrative approach across multiple health disciplines and may necessitate the development of an overall treatment plan. To illustrate a wider scope of practice Dr Hayes outlined 6 key foundations of chronic pain treatment that assumes a structural approach is already in place:
Education – explaining the role of the brain and nervous system interpretation of pain, which commonly has little to do with ongoing trauma. It also incorporates engaging patients in self-management, which over time will help reduce pain intensity. Brainman videos are useful resources to promote understanding about why a ‘definitive diagnosis’ may be elusive.
Biomedical boundaries – setting boundaries around pain medication is key to avoid the treadmill of searching for external solutions e.g. increasing use of opioids or other biomedical approaches, instead focussing on broader treatment approaches. Interestingly this also includes medication deprescribing and the importance of self-management strategies for the patient if surgery is recommended.
Mindbody approaches - identifying unhelpful beliefs and using mindfulness and other techniques to reduce nervous system sensitisation with the aim of reducing pain intensity. Thoughts and emotions impact on our bodies in ways we only recently comprehend, via the gut-brain axis, nervous, endocrine and immune systems. What is empowering is that we can influence how our body responds over time using mindful practices.
Connection - the importance of social interaction is critical for individuals in chronic pain. Loss of connection hurts and this can translate to increased physical pain. Reconnecting with friends, family, workmates and community can become part of a recovery process.
Activity – engaging in activity or exercise appropriate to the individual and their level of disability can help to reduce the pain we experience. Activity in the open air and out in nature also helps calm and has a restorative effect on the nervous system (van den Berg, 2015)
Nutrition – yes what we eat can influence individual experiences of pain. Specifically, nutrition helps to reduce the risk of co-morbidities such as depression, anxiety and obesity. Poor nutrition is also known to contribute to systemic inflammation, which can play a role in chronic pain.
It is important to highlight that this model includes manual therapies such as musculoskeletal therapy, physio or acupuncture. While these options tend to focus on the biomedical aspects of pain, research supports they have a key role as treatment options for chronic pain and certainly prior to more invasive treatment options.
Based on the above recommendations, it is not surprising that a treatment formulation for an individual with chronic pain could be quite comprehensive and involve a number of health care professionals. In our integrative pain clinic, a multi-modality team might include input from a musculoskeletal therapist, a naturopath / nutritionist (that’s where I come in!) and a psychologist. While at first this may seem overwhelming, the important thing to remember is that this model has been shown to have better long-term outcomes than a strict biomedical approach and that is hugely significant when it comes to chronic pain and quality of life.
References:
Hayes, C, 2016. Six Foundations of Chronic Pain Treatment. The Australian Pain Society Newsletter, 6(3), pp. 24-25.
van den Berg, M.M., Maas, J., Muller, R., Braun, A., Kaandorp, W., van Lien, R., van Poppel, M.N., van Mechelen, W. and van den Berg, A.E., 2015. Autonomic Nervous System Responses to Viewing Green and Built Settings: Differentiating Between Sympathetic and Parasympathetic Activity. International journal of environmental research and public health, 12(12), pp.15860-15874.